There was a time when patients with severe pneumonia would loose their life gasping for breath, same was true for people with sudden heart failure. Patients with kidney failure would die because of the effects of build up of toxic products in their blood. Patients whose blood pressure dropped due to a severe infection, did not have any means to keep the blood flow to their vital organ intact, and they would die too. Most of these deaths are preventable, thanks to treatment available in intensive care units all across the globe.
History of intensive care really began in the 1950s during the polio epidemic. Along with other muscles of the body, polio weakens the main breathing muscle, the diaphragm. This caused the patients to die because they couldn’t breathe. A group of courageous medical students in Copenhagen, under the guidance of Dr Ibsen (called father of intensive care medicine), took up the job of manually pushing oxygen and air into those patients’ lungs in 8 hour shifts to keep them alive.
Even before this, various stalwarts including Florence Nightingale suggested putting the sickest patients in the hospital in one single place/ ward so that they could be kept under close observation better. Following the heroic efforts of Dr Ibsen and his team, intensive care units started to get built in Europe and USA. In China and India, it started much later in 1970s and 1980s but has picked in momentum since in providing high quality care.
Currently intensive care is regarded as a separate specialty in most countries and doctors have train for extra years during their post-graduate training to be called an intensive care specialist or intensivist. Similar special training are in place for nursing, physiotherapy, dietetics etc.
What does intensive care do/ organ support – brief idea about cost, both for the healthcare providers and for the patients
Intensive care is “Intensive” care which cannot be provided in a medical or surgical ward
These are the patients whose clinical situation can change in the span of minutes and therefore very close observation is mandatory
Intensive care can provide support for failing organs, all under one roof (ventilator for patients who cannot breath on their own, hemodialysis/ hemofiltration for patients who cannot produce adequate amount of urine for failing kidneys)
There is a concentration of well trained doctors and nurses within intensive care, so that the help is available readily without having to make phone calls.
Intensivists are intensive care specialists with specialist training in carrying on with the functions of different failing organs of human body either with various machineries (ventilator, haemofilters) or with medications.Usually they have done additional training in intensive care mesicine after completing training in anaesthesia or branches of medicine (usually respiratory medicine or but could be acute internal medicine).
They are essentially trained to bridge the period when human body recovers from a life threatening illness until the normal bodily functions resume.
What is sepsis
The international “Surviving sepsis campaign” defines sepsis as inflammation of human body in the presence of infection and it is called severe sepsis when organ functions get affected by sepsis.
Infection from various “bugs” (micro-organisms) have been the cause of human fatality for millions of years and sepsis is the most severe form of adverse effects of infection on human body, when various organ functions are affected by infection. This has been described nearly 2500 years ago by the famous Greek physician Hippocrates and later by stalwarts in medical history (Gallen, Pasteur and the likes).
Patients with sepsis takes up about 1-2 in every 10 ICU beds and therefore this forms a majority of an intensivist’s workload. As described before, when lungs, heart, kidneys cannot function in sepsis, it is the intensivist’s job to run the body function using various machineries and medications giving the body the required time to heal with help of antibiotics.
As sepsis remains one of the biggest killers of humans throughout the world, there have been significant international efforts to improve patient care in and save lives from sepsis. The “Surviving Sepsis Campaign “ was started in Barcelona in 2002 and this has helped improve education amongst doctors and nurses about timely treatment of sepsis and this has already achieved a decrease in mortality by nearly 20%.
Intensivists have been in the forefront of this campaign across the world.Important lessons from this campaign/ related research in the past decade or so
In patients with suspected severe sepsis in hospital, antibiotics should be given as soon as possible (each hour’s delay results in around 7% increase in mortality)
Intravenous fluid should be given as soon as possible
Appropriate sample (blood, urine) should be sent to the laboratory before starting the antibiotics so that it can be shown subsequently what “bug” has caused the problem
Sepsis can result from pneumonia, mengitis, urinary infection or from infection deep inside the body with collection of pus.
If the suspected site of infection is deep seated in the body (in the abdomen or in the joints), appropriate imaging (X ray, scans) should be done as soon as possible so that the pus can be identified and drained by surgery or needle aspiration. This is called “source control” of sepsis – until the pus is extracted, recovery is not possible.
If the initial treatment is not successful, early transfer to a critical care bed improves outcome (i.e. more patients get better)
What is Ventilation/ role of ETT
There are times during a serious illness when it is not any more possible for the patient to continue breathing on his/her own. If not supported by external devices/ ventilator, the patient would be able to breathe and will die. It is in this situation that the ventilators are utilised. These machines support the patient’s breathing until the body recovers enough to be able to initiate adequate breathing.
There are 3 principal causes why a patient may need a ventilator – A problem within the lung (pneumonia, severe asthma etc), a problem in the brain (i.e. the brain is not able protect the upper airway and the lungs can be flooded with secretion – in unconscious patients, head injury etc) or a problem in the breathing muscle.
Depending on the way the disease progresses, the patient may need to have the ventilator very quickly or there may be some time (hours) to predict that this might be needed and the patient and the family members could then be notified in advance of the impending need for ventilation.The ventilation could be delivered by two main ways:
1 Invasive – A tube is passed into airways and is then attached to the ventilator, which in turn, pushes air inside patient’s lungs (image). Usually the patient needs to be sedated (made sleepy) with medications to enable him/her to tolerate the tube in the throat during this type of ventilation.
2 Non-invasive – A tight fitting mask is fitted on to the patient’s face and then the mask is attached to the ventilator, which pushes air inside the patients. The patient should be awake for this type of ventilation
What is BiPAP
This is non-invasive ventilation, where by the patient is fitted with the tigh fitting mask and the mask is then attached to the small ventilator. The patient usually has to initiate a breathing (not often adequate to gain enough oxygen and to flush out the bad gas carbon dioxide), which then triggers the ventilator to push some extra airflow inside the patient’s lung to give an adequate breath.
If the patient is not adequately conscious, it is not safe to use this type of ventilation. Similarly, in severe failure in breathing, this is often unsuccessful.This is particularly very useful in respiratory (breathing) failure related to COPD (chronic obstructive pulmonary disease).
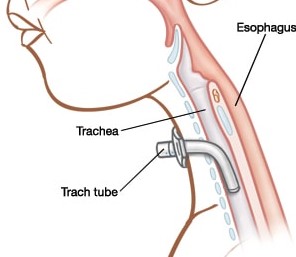
(Tracheostomy) As depicted in this image here (Source:uofmchildrenshospital.org) the endotracheal tube cannot be left in the airway for long. It is usual practice that the patient who cannot do without the ventilator after 10-14 days, should have a tracheostomy instead (see figure). If kept in for long time, the endotracheal tube can cause damage to the trachea.
Additionally, this allows to stop the sedative drugs that were being used to make the patient tolerate the endotracheal tube. The patient can then be mobilised, sat in a chair and this process of coming off sedation and mobilisation aid in their recovery. Some patients, however, will have to be kept sedated even with tracheostomy if their breathing is still severely impaired.
New modalities – ECMO
Lungs provide oxygen to the blood and remove the harmful carbon dioxide from blood stream. There are situations where even the best ventilators and the best intensivists fail to support the breathing of the patient because the lungs are in so badly damaged, at least temporarily. Often even the worst affected lungs would recover to make the patient better again if he/ she could be supported for a few days to few weeks with an alternative strategy to supply oxygen to vital organs. And here come the place for ECMO. Where ventilator fail, ECMO can do the job of mixing oxygen in the patient’s blood and also of removal of the waste product carbon dioxide.The full form of ECMO is Extra Corporeal Membrane Oxygentation.
One or two large catheters are placed in the vein, blood is removed from the patient’s body through this catheter and is passed via the oxygenator (which mixes the oxygen into the blood) and then the oxygen mixed blood is returned to the patient’s body by the catheter again. One can call this “lung dialysis”.
Forms of kidney support
About 30-40% patients in ICU, have some form of damage to their kidney function. Approximately 5% patients in ICU have such a severely affected kidney function, that they have to be given artificial support to carry out the function of the kidneys.
Venous access: The doctors need to insert a large bore venous catheter in eithr the neck vein, vein just below the collar bone or in the veins of the groin. This catheter is then used to take blood out of the patient’s body, run it through the hemodialysis/ hemofiltration machine and then returned back to the patient’s body again after purification.
Sometimes, adequate flow cannot be generated and the line may need to be changed. These lines can be potential source of entry of infection into patient’s body and therefore meticulous care needs to be taken whilst handling the line
Hemodialysis, Hemofiltration, Hemodiafiltration or SLEd (Sustained Low Efficiency Dialysis) are various forms of renal replacement therapies that can be used by intensive care units depending on the facilities available. None have been proven to be better than the other in critically ill patients and the choice depends on the patients clinical state as well.
What happens to patients who need kidney support
As these are amongst the sickest patients in the ICU, understandably, the mortality rate in this group of patients are fairly high at 40-50%. Of the patients who recover, about 10% need long term hemodialysis (HD), and the chance of needing HD is higher in patients who had kidney disease before, or who have diabetes or high blood pressure. In about 60% of the survivors, kidney function completely goes back to normal.
Is there any particular supporting device for liver in ICU
At the moment, there is no liver support device available like the hemofiltration device is for the kidneys. When a patient is admitted with severe liver failure, the intensivist’s job is to keep other parts of the body as stable as possible and give the liver a chance to recover. In very severe liver failure, the only successful treatment is transplant if the facilities and a suitable donor organ are available. Some new devices (ELAD) are under research currently but are not in regular clinical use
Stroke/ neurological disease related intensive care
Brain plays a few important roles in breathing. Firstly, it controls the smooth breathing pattern that we all have in good health. Secondly, it has got a role in swallowing saliva or other secretion within the mouth cavity and at the same time protecting the airway from these secretion so that a open airway is maintained. Therefore, when brain does not function well enough to do these jobs well, it is safer to put the patient on a ventilator; not doing so can put the patient’s life in danger.It is not uncommon for patients following certain kinds of stroke, severe epileptic fit, encephalitis, brain injury or patients after brain surgery to be kept on a ventilator.
During treatment, it is of paramount importance to keep their brain in the best possible physiological environment. This can be achieved by ensuring good blood supply to various parts of brain tissue. For this, precise control of blood pressure is mandatory. Additionally, the intensivist needs to ensure that the pressure within the skull vault is not too high, which will directly impair blood supply to the brain and the brain tissue would be permanently damaged.
Therefore, it is important to have specialised monitoring device and specifically trained personnel to treat these patients. There is emergence of specialised intensive care units called neuro-ICUs which can deal with complex and different type of monitoring needs for patients with brain disease in need of organ support.
In addition to the usual organ support infrastructure, these units also have various different forms of intracranial pressure monitoring device and any change in the intracranial pressure should be promptly managed to prevent any permanent damage to the brain. These units also have immediate access to a neurosurgeon.
Forms of cardiovascular support
A well functioning heart and blood vessels which can respond to changes within human body (lack of fluid, high temperature, infection etc) is needed to maintain blood flow to all the vital organs. Essentially under physiological stressful situation, a strong heart pumps more vigorously and the blood vessels squeeze hard to narrow down to keep up the boold pressure. However, in severe sepsis or in blood loss and in some other disease states, these normal responses of heart and blood vessels could be lost and then the organs (including the brain and the heart itself) come under the risk of being deprived of blood supply and the person will die.
It is in this situation that an intensivist can use medications (Noradrenaline, Dopamine etc) firstly to squeeze the blood vessels to keep the blood pressure at a near normal level and then can also use some other drugs (Dobutamine, Levosemendan, Milrinone) to make the heart pump stronger than it could have done on it’s own. It is also important to maintain adequate amount of fluid in the patient’s body and the intensive care doctors are trained in using various monitoring devices and clinical examination to achieve this.
Without cardiovascular support, all other interventions will fail to keep the patient alive.
Role of different IV lines
During an intensive care stay, the patients need a combination of the following
Intravenous fluid
One or two different continuous intravenous intcardiovascular drugs
One or two drugs for keeping the patients sedated
Often patients even with no diabetes have high blood sugar during serious illness – therefore continuous infusion of Insulin
Frequent intravenous antibiotics
In small group of patients, intravenous nutrition would be needed
Depending on the underlying disease, infusion of some other drugs
Therefore, it is not uncommon to have 5 or 6 different intravenous infusions running continuously in these patients. Some of these drugs cannot be given through a peripheral smaller vein and to be given in a vein close to the heart. Additionally, they have to be given a very precise rate (slight increase or decrease of these drugs can have disastrous effects on the patient).To achieve these goals, doctors do the following:
Insert intravenous catheters in larger veins (usually in the neck, but also could be in the groin or just under the collar bone). These are called central venous catheters.
These catheters have 3-5 different ports, so a number of drugs can be given through these catheters.
Use electronically controlled syringe drivers which could give these drugs at the rate chosen for the patient – a ptient can be attached to 5-6 syringe drivers, each syringe containing a different drug
A nurse is employed for only one (at the most 2) patient so that these syringe drivers could be kept under close observation, they need changing when drug runs out and there cannot be any delay in these changes.
Occasionally, if the number of drugs could be more than what could be given via these catheters. In these situations, a peripheral venous channel is placed as well.
These central venous catheters could be easy source of infection if not looked after properly and therefore every ICU should follow internationally agreed guidelines to look after these catheters and change them in case any sign of infection appears, as thses infections could be serious.
Why do people look sleepy/ kept asleep in intensive care
As mentioned before, patients who are ventilated, need an endotracheal tube and it is difficult to be comfortable with a tube in one’s airway. To keep patients comfortable, often some amount of sedation is used.Additionally, all the interventions (putting big intravenous catheters etc) and the noise in the ICU can have problems with the psychological processes of the patients and a little bit of sedation helps this
However, it is well recognised time and again in research studies that too much of sedation has ill effects and the intensivists and the ICU nurses always try to keep the sedation to minimum possible level.Good medical treatment, like other things in life, is all about having the right balance, not too much and not too little.
Why sometimes it takes a long time (Catabolic state/ CPN) for patients to recover in intensive care units
It is well recognised that in the initial phase of a critical illness, a patient looses enormous amount of muscle bulk. Often nerves supplying muscles get affected as well. This means that movement of limbs as well as making effective breathes using the breathing muscle become difficult. Therefore, understandably, patients who get these ill effects of their critical care illness, take much longer to recover and often need weeks of stay in the ICU. This prolonged stay can get punctuated by intermittent infection (as the immunity is already low and chance of picking infection in ICU is always high), making the stay even longer.
Why often patients need CT scan or other scans
There are times when it becomes unclear why a patient in ICU is having a temperature or where is a possible source of internal bleeding. It is often impossible to find the cause without doing detailed scan and it goes without saying that without finding the correct cause, no appropriate treatment can be given.
A decision to do a scan for a ICU patient is taken is taken extremely seriously as transferring a patient from ICU to the scanner is associated with risks with the patients attached to multiple infusion pumps and the ventilator. A well trained nurse and a doctor should accompany the patient to the scanner.
How many actually survive/ pitfalls of statistics
The patients in the ICU are the sickest in the hospital. Understandably, a significant proportion of them do not survive despite all the organ supports that they receive in ICU. There is large amount of ongoing research across all the continents to improve this. One things has been proven beyond doubt that if the harmful side effects of many treatments within the ICU can be reduced, then the mortality rate could also be reduced. That is where rigorous quality control within ICUs and continuous training become so important.
A simple guide to mortality rates from various disease state or organ support is given below:
Severe sepsis [20-30%]
Patient needing ventilation [15-30%]
Patients needing kidney support(dialysis/ filtration)[40-60%]
Patients with acute liver failure[30-40%]
Patients with severe head injury[30-40%]
Patients after major emergency abdominal surgery[15-20%]
Like any other statistical value with global significance, this numbers are an indicator only and can vary country to country. These are value derived from ICUs in developed countries and from units interested in participating research studies and therefore if one looks at the wider picture, it is expected that the rates are even higher.
Another important point is that with increasing age, mortality goes up. Number of failing organs also significantly increases the chance of death.
It is always helpful to if a discussion takes place between the intensivist and the patient’s family members at the beginning of ICU stay and daily thereafter outlining the overall clinical situation with a rough idea about possible outcome. This can prevent any unrealistic and false hopes.
Antibiotics
The greatest medical discovery of the nineteenth century are the antibiotics. Before Penicillin was discovered, people would die of simple infection and pneumonia was ineedd the “captain of the men of death”. We do not see pneumonia is a certain killer anymore thanks to the antibiotics.
However, the last few decades have seen increasing number of bacteria that do not get killed by even the strongest of antibiotics. MRSA, VRE, CPE are description of these deadly superbugs who have learnt fight with the antibiotics and is hard to kill.
A few reasons for emergence of such antibiotic resistant bacteria are:
As bacteria get exposed to antibiotics, changes happen in genetic makeup of bacteria giving them structural changes that do not allow for the antibiotics to be effective
Sometime these genetic changes take place spontaneously in bacteria without any exposure to antibiotic
Wrong choice of antibiotic kills the weaker bacteria, keeping alive the more number of “bad” ones and with increasing numbers, they can be more harmful
Rampant use of antibiotic in animals, both for infection and as growth stimulant has caused formation of resistant bacteria within animal body (which then get consumed by humans) and also in the atmosphere – this is one of the biggest threats.
Intensive care, especially in the Indian subcontinent, has become a minefield of such resistant bugs for various reason. In a recent report 57% of a fairly harmful bacteria were found to be resistant to the strongest available antibiotics.
Possible solutions:
Choice of antibiotics has to be done wisely, especially in the ICU in conjunction with results from microbiology laboratory (which tells us which antibiotic to be used for specific infection and bugs)
Reducing use of antibiotics rampantly within primary care by local doctors – more the antibiotics use, more the resistance
Reducing uncontrolled antibiotic amongst animals
Within hospitals, strict adherence to infection control protoclol (hand washing before and after patient contact, cleaning medical equipment appropriately, hospital wode antibiotic protocol)
Discovery of new antibiotics
International experts otherwise predict that within the next 2-3 decades, we will run out of options and people will start dying from simple infections again like what used to happen before 1930s before the discovery of Penicillin.
What is the importance of safety procedures in ICU
Importance of this cannot be emphasised enough. Running a well functioning ICU is like running a fleet of airliners in a safe a effective ways. The senior doctors and nurses along with senior hospital management need to ensure:
Doctors and nurses with appropriate training are employed, otherwise a small error in judgement can have catastrophic effect
All the equipments are serviced regularly and everyone knows their utility at a level appropriate for them
There are 1-2 ward rounds daily where the seniors doctors and nurses are present including other important member of the team
A pharmacist is essential as they keep a check on drug dose and duration etc
Regular training in policies and procedures within the unit is a must to keep everyone uptodate
Rigorous infection control measures should be in place, the last thing a critically ill patient needs is another infection from patient in the next bed through the hands of doctors/ nurses/ physiotherapists/ porters/ cleaners/ visitors.
Using easily implementable care bundle for central venous catheters, ventilation care etc.
Close liaison with the microbiology department so that the patients could get right antibiotic at the right time
A culture within the ICU where people can continuously discuss with each other how to improve matter even further
We do not want our aeroplane to crash and this can happen due to a minor lapse in the safety procedure before that the aircraft started flying; similarly we don’t want a single patient to die because of safety procedures not being followed witin ICU.